Tackling healthcare claims can sometimes feel like scaling a steep hill, with heaps of paperwork and drawn-out delays bogging you down. That’s where EDI 837 steps in to save the day. This HIPAA-supported system revolutionizes the traditional claims process, making it quicker, reducing errors, and trimming down on administrative expenses. The 2024 CAQH Index report highlights a huge win for the industry—$222 billion in savings—and shows providers cutting about 5 minutes per claim with EDI claims automation. Whether you’re overseeing a small clinic or a large hospital, getting a solid grasp on EDI 837 healthcare claims processing is crucial for keeping things running smoothly and staying in line with HIPAA EDI standards. As of today, Wednesday, August 13, 2025, at 12:43 PM IST, this guide is brimming with the latest tips to set you on the right path.
Deep down, EDI 837 healthcare claims processing is a straightforward electronic tool that takes the hassle out of sending medical billing claims to insurance companies or government agencies. this beats the ANSI X12 transaction kit and ensures that the patient's information, diagnosis and fees are accurately assigned according to the HIPAA 5010 rules. Switching into this method from paper increases speed and harassing safety, lost files and slip-ups excluded from the image. This health care system is an important part of the EDI work flow, especially if you are surprised by 837p against 837i that interfere with or work to comply.
EDI 837 bends to meet the different needs of healthcare with three main groups, each playing a key role in making EDI claims automation hum along:
837P – Professional Claims: Crafted for docs or therapists, it groups up with the CMS-1500 form to deal with outpatient care.
837I – Institutional Claims: Built for hospitals, it manages both inpatient and outpatient claims and may juggle up to 25 prognosis codes the use of the UB-04 form.
837D – Dental Claims: Shaped for dentists, it speeds up submissions for things like cleanings or fillings.
So, what sets 837P apart from 837I? It’s pretty simple—837P focuses on one-on-one patient care, while 837I takes on facility-based services, both feeding into the healthcare EDI workflow.
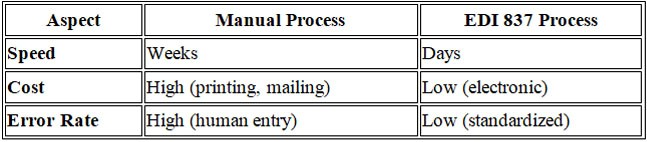
Switching to EDI 837 healthcare claims processing offers some tangible benefits. The 2024 CAQH Index notes $222 billion in savings, and it transforms weeks of waiting into just days for payments to arrive. It reduces errors with reliable data and cuts costs linked to paper, printing, and mailing. Plus, encrypted transmissions keep patient information safe, meeting HIPAA EDI compliance and sparing patients from billing surprises.
Picture an EDI 837 file as a well-organized binder, assembled with segments in the ANSI X12 format that keep the healthcare EDI workflow on course:
For 837I, that 25-diagnosis-code limit is a huge asset for dealing with complicated cases.
Here’s how EDI 837 healthcare claims processing unfolds from start to finish:
A quick diagram of this cycle—from enrollment (EDI 834) to payment (EDI 835)—helps it sink in for those who like to see things laid out.
EDI 837 weaves in a large system, combining EDI 834 (which handles eligibility) and EDI 835 (for payment) to create a smooth EDI workflow for the health care system. Imagine this way: You start by confirming the coverage with 834, then send claims using 837, and finally paid by 835.
Incorporating EDI claims automation with software linked to EMRs reduces rejections, saving that 5 minutes per claim noted by CAQH. It’s a practical boost to your healthcare EDI workflow efficiency.
A straightforward flowchart or infographic can really drive home the cost savings. Here’s a quick look at the difference:
Take Harmony Clinic, a mid-sized practice that was struggling with sluggish reimbursements. Before they brought in EDI 837, they were dealing with a 20% rejection rate and payments that took 45 days, putting a real squeeze on their cash flow. Once they switched to EDI 837, rejections fell to just 5%, payment times dropped to 20 days, and they saw a solid 15% boost in reimbursement rates. On top of that, they cut their admin time in half—freeing up staff to concentrate on patient care.
EDI 837 Healthcare claims that the treatment of HIPAA follows 5010 standards and protects data. Regular training for your team and periodic revision is the best way to combine HIPAA EDI SAMPAGE..
EDI 837 healthcare claims processing sets the stage for a smooth, rule-abiding healthcare operation. With a hefty $222 billion in savings and 5 minutes cut from each claim, as highlighted in the 2024 CAQH Index, it’s a wise move for any practice to jump on board. Putting effort into EDI claims automation, training your team well, and relying on dependable tools can tidy up your workflow, cut down on rejections, and lift your reimbursement rates. Whether you run a cozy clinic or a bustling hospital, this approach gives you a leg up in the game. Dig into more tips at HIPAA.gov or CAQH Index, and take a look at what we offer on our services page.